Affected women with PMS should keep a PMS diary for at least 2 cycles recording their symptoms. A Daily Record of Severity of problems (DRSP) chart can be accessed at HERE.
Further information on PMS can be accessed at www.pms.org.uk
If you prefer to record your symptoms on an app - a free PMDD app (ME vs PMDD) is available :
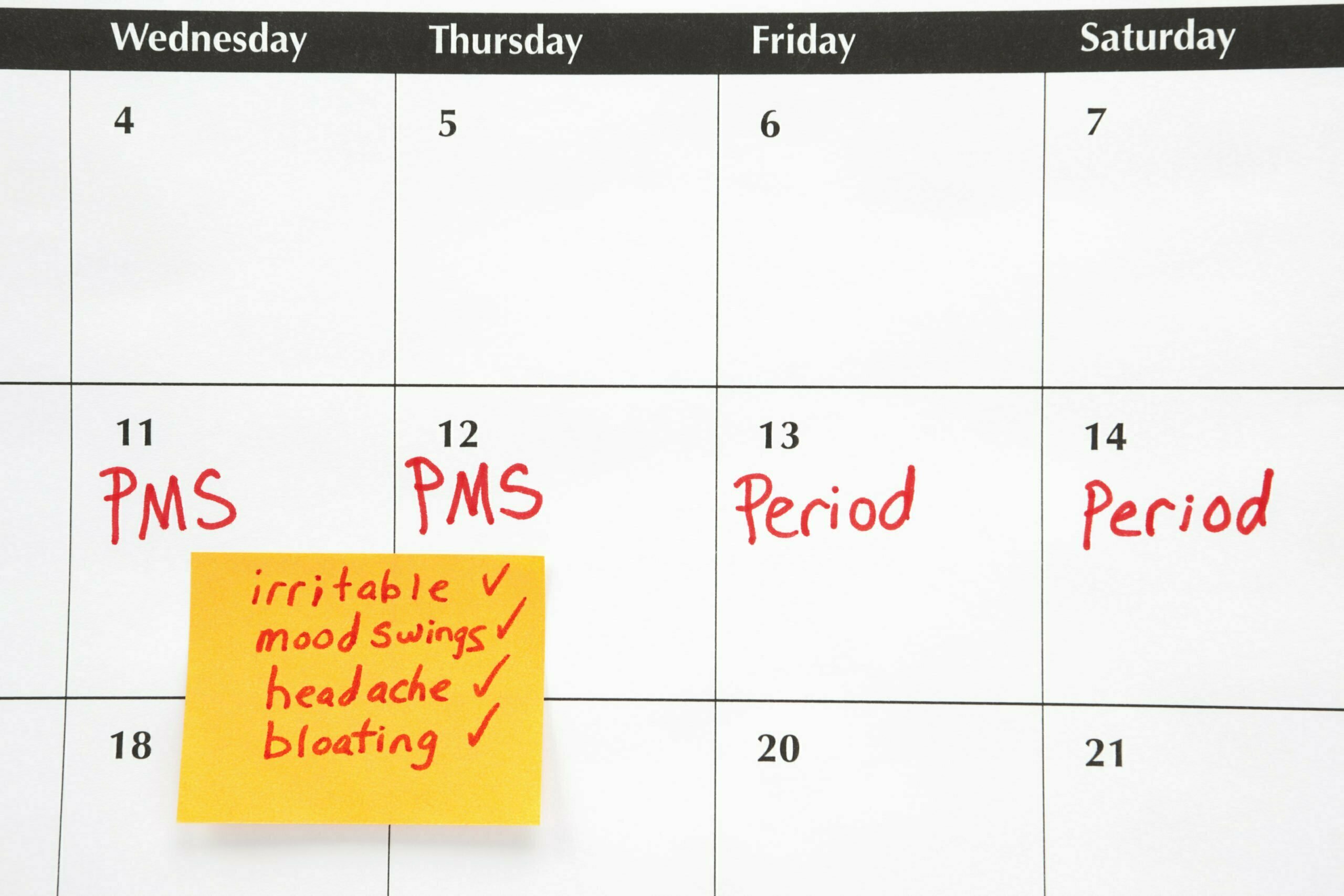
Symptoms can be physical or psychological, which may impact your quality of life.
Physical: bloating, breast tenderness, headaches and weight gain. Some women experience worsening of migraines, asthma and epilepsy attacks in the premenstrual phase.
Psychological: depression, mood swings, tension, increase anxiety, irritability, food cravings.